The microbiome of cancer
During the course of evolution, animals, including humans, developed a profound mutualistic relationship with a variety of different microbes. The diversity of our microbial “friends” is immense and they occupy almost the entire body. For instance, scientists found that a change in microbiome composition in the gastro-intestinal tract (gut microbiome) could lead to all sorts of diseases, from simple diarrhoea to different kinds of more serious illnesses, such as arthritis, inflammatory bowel disease and even depression.
In addition, a healthy gut microbiome is believed to educate and boost our immune system and thus contributes to a healthy and long life. As of late, the connections between microbiome and cancer are being drawn. Although, this area of research is still in its infancy, it turns out that local and distant microbiomes are involved in the initiation, promotion and progression of cancer. The local microbiome is near the solid tumour, and the distant microbiome is in other organs, such as the gut (Jain et al. 2021).
The odd beginnings of microbiome of cancer research
The impact of some microbes on the development of cancer has already been known for years. In 1911, Peyton Rous discovered a virus called Rous sarcoma virus (RSV) that induces sarcomas (malignant tumours that arise from connective tissue such as bone) in chickens. After that, the hunt for tumour-promoting microbes began, and a multitude of other microbes were shown to induce cancers, such as the Epstein-Barr virus (EBV), which can induce nasopharyngeal carcinoma as well as Burkitt lymphoma, or Helicobacter pylori that can induce gastric cancer.
While those examples reflect the negative impact of microbes, going back before Peyton Rous, in the late 19th century, William Coley treated sarcomas by injecting a mixture of bacteria, called Coley’s toxin, and showed that microbes can have a positive effect on a sarcoma patient’s outcome.
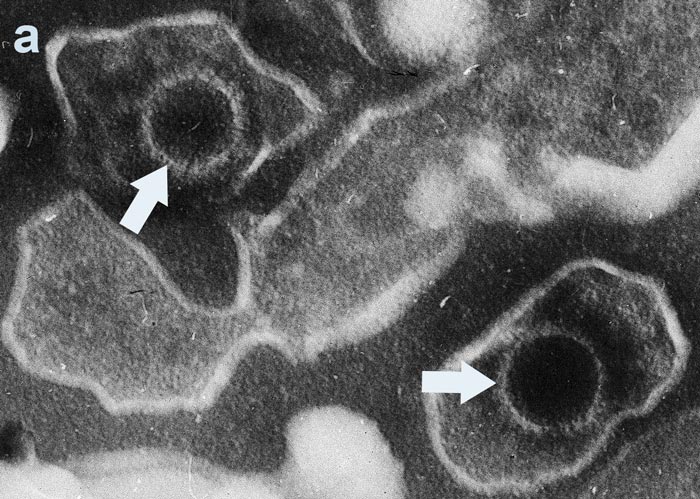
Image 1: a) Epstein-Barr virions and b) Helicobacter pylori, c) William Coley (center), 1892.
The continuation of microbiome of cancer research
More than a century later, with advances in genome sequencing and metagenomics, we finally began to identify the microbes responsible and started to understand the mechanisms by which microbiome can influence cancer development. Even though these mechanisms largely remain elusive, it is suspected that microbes can influence cancer development directly by modulating signalling pathways and metabolic circuits of cancer cells, as well as indirectly by modulating anti-tumour immune responses (Zitvogel et al. 2016).
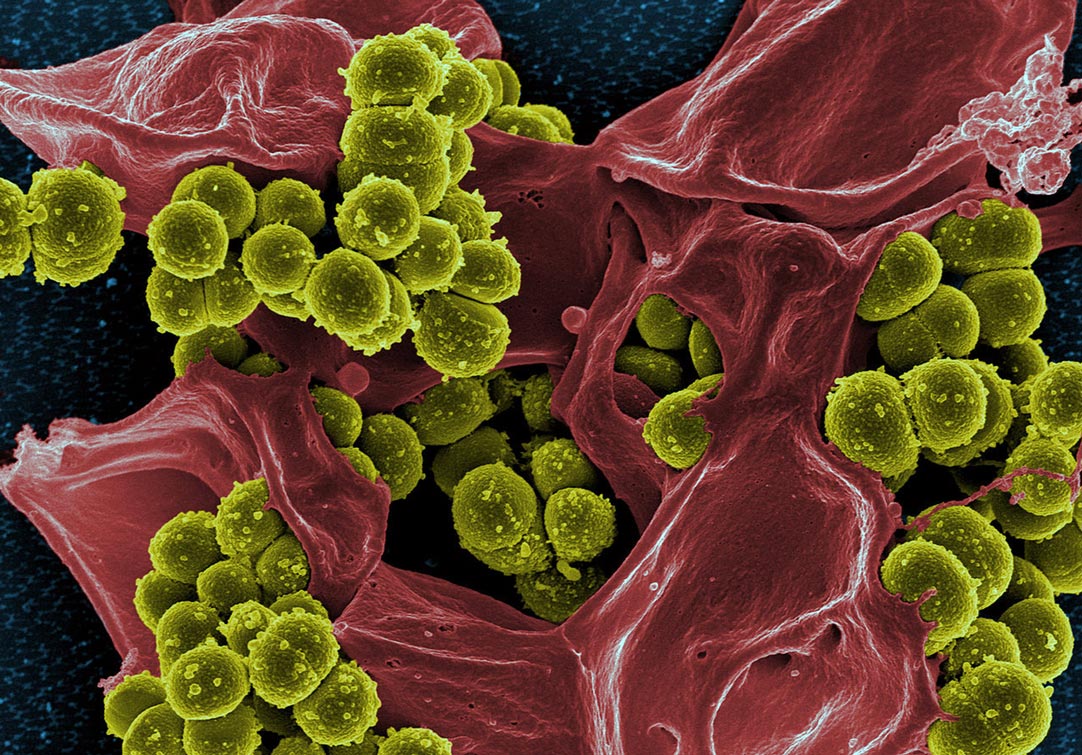
Bacteria are ubiquitous throughout the human body and inhabit almost every tissue, but they are most prevalent in the gut. Each organ or tissue has a differently composed microbial community as each organ or tissue represents a distinct environment. Tumours are no exception. Tumours, and their microenvironment, are significantly different from the tissue from which they arise and thus are inhabited by specific types of microbes. The most characterised microbes in this case are bacteria. For example, it is known that Fusobacterium nucleatum, Lactobacillus iners and Streptococcus infantis are found in breast cancer samples, and Citrobacter freundii, Klebsiella pneumoniae and Enterobacter asburiae in pancreatic cancer. Furthermore, some studies suggest that most of the bacteria reside inside tumour cells, which implies that metastasising tumour cells carry their bacteria along with them. This in turn implies, although not proven, that when tumour cells arrive at a distant organ or tissue, their mutualistic companions help them to construct a new niche in which a new metastatic tumour will flourish. Interestingly, the tumour also induces a dysbiosis in the residing tissue, meaning that the normal composition of the microbial community of the given organ or tissue is disturbed. Proof of the relationship between cancer and microbiome comes from faecal microbiota transplantation (FMT) experiments, in which the microbiome from patients with colorectal cancer (CRC) was transplanted into germ-free mice. Those mice then developed CRC, which proved the carcinogenic potential of CRC patient’s gut microbiome (Figure 2).
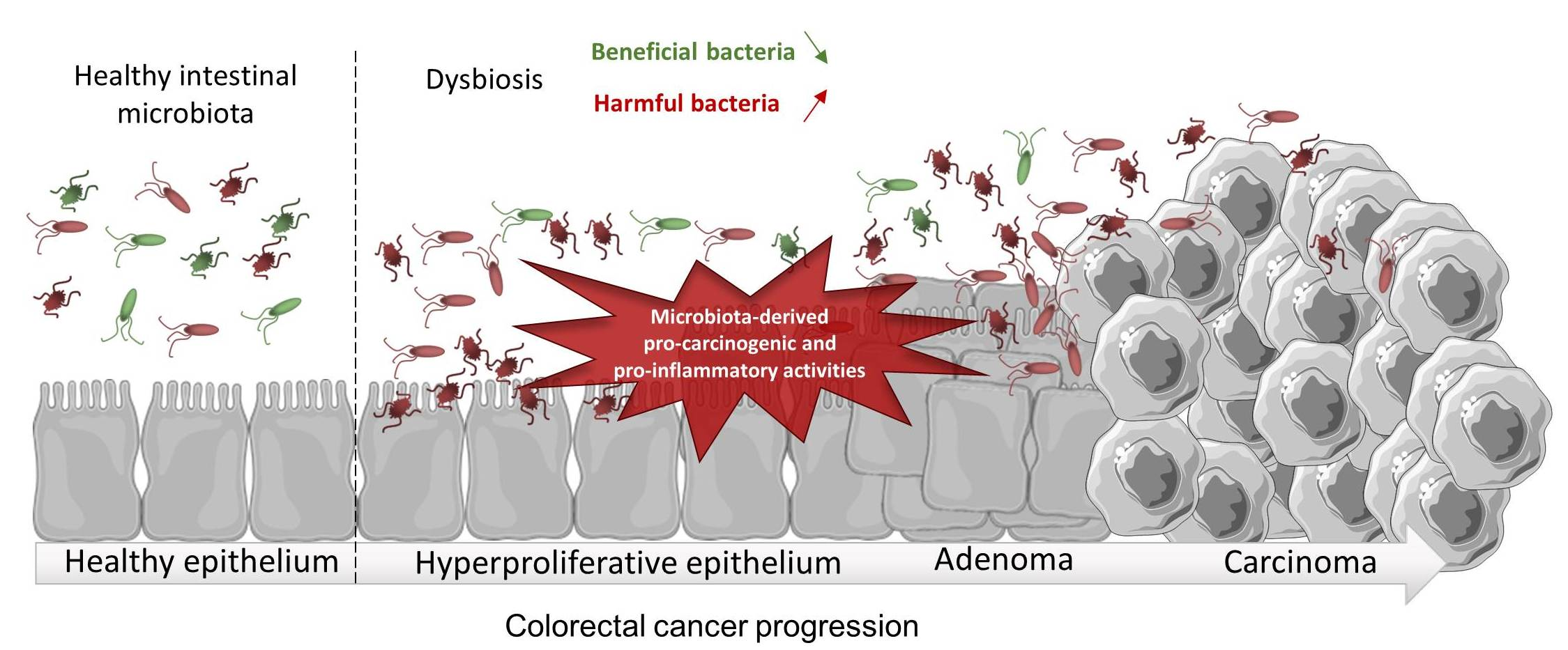
Figure 2. Alteration of composition of colon bacteria and its influence in development of colorectal cancer.
Could a ‘cancerous’ microbiome from a specific type of cancer support the development of the same cancer in a different organism? This has been shown for different types of cancers; for mice with breast cancer, hepatocellular carcinoma (affecting the liver), pancreatic cancer and melanoma, all with similar results. The gut microbiome seems to influence the initiation of cancer in distant, seemingly unrelated, parts of the body. The mechanisms behind this are still unknown, but there are many hypotheses that could explain both the positive and negative influence of the microbiome on cancer (Marshal et al. 2021; Nejman et al. 2020; Chen et al. 2019).
Direct influence of the microbiome on cancer cells
There are several ways microbes could affect cancer cells. The obvious way is that they could restrict the availability of nutrients by using them for their own metabolism. However, microbes also secrete certain metabolites, such as amino acids, lipids or proteins, that cancer cells in turn can use for their own energy metabolism, or that can bind to receptors on the surface of cancer cells and affect their intracellular proliferative signalling. Furthermore, microbes can alter the tumour microenvironment by changing pH or producing reactive oxygen species (ROS). ROS can induce activity of NF-κB (transcription factor involved in regulating immune responses) and subsequently activate the expression of pro-inflammatory factors that favour cancer growth. Additionally, bacteria can directly bind to cancer cell receptors such as the G-protein coupled receptors (such as EGFR) and thus activate proliferative signalling. As mentioned earlier, some of the bacteria reside inside cancer cells and thus can be directly implicated in metabolism and signalling pathways by secreting or absorbing different factors (Marshal et al. 2021).
Influence of the microbiome on the immune system
Along with the direct mechanisms described above, the microbiome plays a crucial role in the development of a healthy and strong immune system, regardless of cancers. There are a number of studies showing that germ-free organisms are more susceptible to all sorts of illnesses, including cancer. And yet, again, the mechanisms involved remain poorly understood. There are several possible mechanisms that are not mutually exclusive.
First of all, microbes produce metabolites that can enter the bloodstream and modulate the activity of immune cells from a distance. For example, butyrate is known to be essential for the survival and memory of CD8+ cytotoxic T-cells. Butyrate and acetate can also activate Treg cells, and thus positively affect tumour growth.
Another mechanism may involve pathogen-associated molecular motifs (PAMP) that can induce the innate immune system; macrophages or natural killer cells that are important in eliminating early-stage tumours, as well as educating lymphocytes by presenting tumour-specific antigens.
There’s yet another possible way of stimulating lymphocytes to attack tumour cells. Some of the microbes’ antigens have a high homology with certain tumour antigens. This is a phenomenon called ’antigen mimicry’. So, there’s a possibility that lymphocytes ’learn’ how to attack tumour cells, even if that tumour type has never existed in the body (cross-reactivity). Even though it is known that homologies between microbial and tumour antigens really do exist, this mechanism still remains unproven (Figure 3) (Zitvogel et al. 2016).
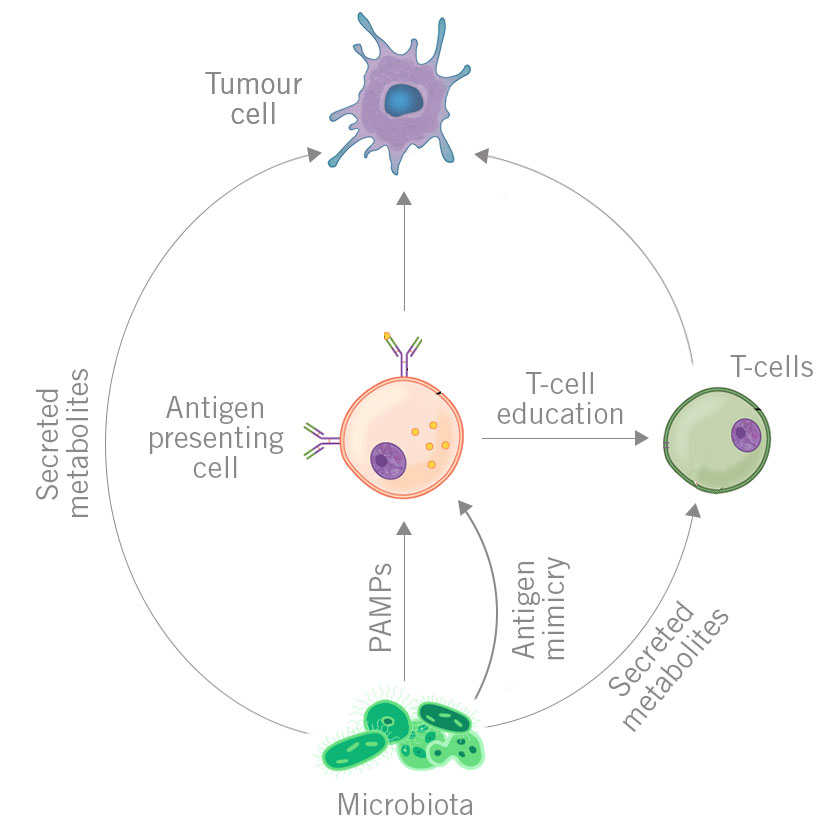
Figure 3. Mechanisms of influence of distant microbiome on cancer. Each type of mechanisms is labelled with different colour.
Conclusion
Microbes are of immense importance to general health and tumour development in humans. Some of them promote tumour development, and others do the opposite by teaching our immunity how to react if a tumour appears in the first place. All of this underscores the importance of a well-balanced composition of bacteria in different organs of our bodies.
By Matko Tudor and Dr Andreas Ebertz
Did you like this article on the microbiome of cancer? Then subscribe to our Newsletter and we will keep you informed about our next blog posts. Subscribe to the Eurofins Genomics Newsletter.








2 Comments